As a specialist in gestational diabetes nutrition, I get a lot of questions about blood sugar and pregnancy.
Gestational diabetes is controversial. It’s complicated. And there’s a lot of misinformation out there.
I do my best to address the controversies in interviews and with participants in my online gestational diabetes course, but since I’ve been receiving more and more inquiries in my inbox from fellow healthcare professionals, I wanted to dispel some gestational diabetes myths head-on right here on the blog.
I’ll also be attending some midwifery conferences this year (including one this weekend), and I figured this resource would be a helpful place to refer practitioners if they have questions.
Given the medical interventions that are commonly pushed on women with gestational diabetes (believe me, I’m also disheartened by the over-medicalization of pregnancy and birth), it’s important to understand the science behind high blood sugar and pregnancy.
My goal is to help moms and practitioners make better decisions – based on fact, not fear – so they can have the healthiest pregnancy possible.
9 Gestational Diabetes Myths
Myth #1: Blood Sugar Levels are Naturally Higher In Pregnancy
There’s a lot of misinformation floating around about blood sugar levels in pregnancy. Some think that gestational diabetes is a “diagnosis looking for a disease.” In other words, they believe that blood sugar levels naturally go up during pregnancy, so there’s nothing to worry about.
Some practitioners don’t even test for gestational diabetes and just tell their patients to “eat healthy” under the assumption that any rise in blood sugar is just a normal phenomenon of pregnancy.
Unfortunately, that’s not true. Research has looked at blood sugar levels in normal, healthy pregnant women and found that blood sugar levels consistently trend 20% lower than blood sugar in non-pregnant women. (Diabetes Care, 2011)
Read that again: 20% LOWER.
This is why there’s so much confusion when you hear about the “low” blood sugar targets for gestational diabetes compared to non-pregnant blood sugar goals. Your body is literally OBSESSED with keeping your blood sugar as low as possible in pregnancy.
A research study that explored patterns of glycemia in normal pregnancy across 11 studies published between 1975 and 2008 found:
“The most compelling finding from our review of the available literature is that glucose concentrations during normal pregnancy in the absence of obesity are lower than the current suggested normal therapeutic targets. [T]he weighted mean pattern of glycemia reveals an FBG of 71 ± 8 mg/dL, followed by 1- and 2-h PP glucose concentrations of 109 ± 13 and 99 ± 10 mg/dL, respectively, and a 24-h glucose of 88 ± 10 mg/dL. These weighted mean values are appreciably lower than the currently recommended therapeutic targets…” (Diabetes Care, 2011)
Myth #2: Mildly Elevated Blood Sugar is Nothing to Worry About
What if your blood sugar is only slightly elevated, by around 5-10mg/dl above targets? Certainly that’s not a problem, right? I wish that was the case, but researchers have observed that some of the problems associated with gestational diabetes can occur even in fairly “mild” cases, like having a baby with high insulin levels or one who is abnormally large at birth.
The landmark Hyperglycemia and Adverse Pregnancy Outcomes study (HAPO), which studied 23,316 women with gestational diabetes and their infants, found that even mildly elevated fasting blood sugar levels were linked to high insulin levels in infants at birth and macrosomia (Int J Gynaecol Obstet. 2002).
For example, women with an average fasting blood sugar of 90mg/dl or less had a large baby 10% of the time, compared to 25-35% in women whose average fasting blood sugar was 100mg/dl or higher. A more recent study out of Stanford found a significantly higher risk of congenital heart defects in babies born to women with mildly elevated blood sugar (even below the diagnostic criteria for gestational diabetes). (JAMA Pediatrics, 2015)
The bottom line is: your blood sugar levels in pregnancy matter. Clearly, the adverse “fetal programming” typically attributed to gestational diabetes may be occurring to mothers who experience only slightly elevated blood sugar. This means what you eat matters, the amount (and quality) of carbohydrates you eat matters, the amount of sugar you eat matters, the amount of nutrients that naturally regulate blood sugar matters, the amount of sleep you get matters, the amount of exercise you get matters, etc, etc, etc.
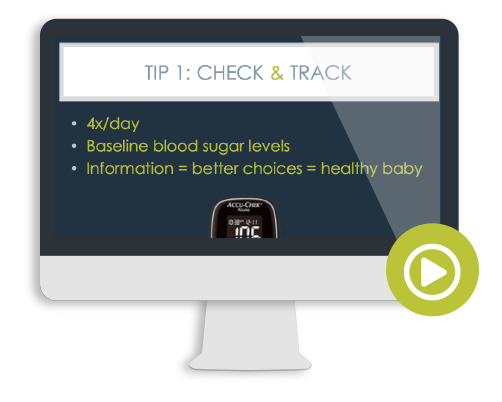
If your blood sugar is elevated, it means you need to get curious about why and how to fix it (meaning using food, exercise, possibly supplements and other lifestyle tweaks… and if those aren’t enough, medication or insulin). I walk you through the basics in this free 3-part video series if you’re interested to learn more.
Myth #3: Gestational Diabetes Magically Appears Out of Nowhere at the End of Pregnancy
While it’s true that insulin resistance rises in the second half of pregnancy (as a normal adaptation, so your body can shunt as many nutrients to your rapidly growing baby), gestational diabetes is rarely something that just “appears” with no warning signs.
As research into gestational diabetes has advanced, researchers noticed that rates were rising right alongside higher rates of prediabetes and type 2 diabetes in the general population. This led some to believe that gestational diabetes wasn’t entirely a phenomenon of placental hormones and pregnancy-induced insulin resistance, but undiagnosed prediabetes that was “unmasked” (meaning finally tested for) during pregnancy.
One study that measured average blood sugar in early pregnancy via a test called hemoglobin A1c (or just A1c for short), found that an elevated first trimester A1c was 98.4% specific for detecting gestational diabetes. (Diabetes Care. 2014) Coincidence? The first trimester is before the onset of insulin resistance and when blood sugar levels in pregnancy are typically lowest.
Another study found an early pregnancy A1c of 5.9% or higher is linked to a 3-fold higher rate of macrosomia (large baby) and preeclampsia. (J Clin Endocrinol Metab, 2016) Some researchers are calling for universal screening by this method, as it’s both accurate and non-invasive (and A1c can simply be added to your routine early pregnancy blood panel). Plus, if you identify a problem now, you can actually be proactive and DO SOMETHING about it, rather than just wait around until the 24-28 week glucola screening.
PS – In-the-know docs will test your first trimester A1c as an alternate way to screen for GD. Anything in the prediabetic range (5.7% or above) is considered gestational diabetes. You can also request your doctor check your A1c if it’s not on their radar. That’s what I did.
Myth #4: The Glucola/Glucose Test is Fail Safe: If You Pass the Glucose Test, You Can Eat Whatever You Want
There’s a lot of black and white thinking when it comes to gestational diabetes. You might think that as long as you pass your GD screening test you are fine and can eat whatever you want. (I know a fair number of women who will go out for a celebration milkshake when they pass.) On the other hand, if you fail, suddenly the sky is falling! Now you’re “high risk”, will have to be on insulin, will have a large baby that will get stuck during delivery, and then you’ll be induced or need a C-section, etc, etc.
And – full disclosure – I entirely understand these fears, especially that your birthing options could be limited because of a label. If your healthcare providers fall into this fear-based thinking and have never seen gestational diabetes well-managed, they don’t always understand that there can be another way and they immediately go to worst case scenario.
It’s important to understand that blood sugar is on a continuum and the relative risk of complications relies on your blood sugar levels, not a label!
Plus, the glucose tolerance test (aka the glucola) is not perfect. Some women with an elevated first trimester A1c, indicating prediabetes, will pass the glucola despite clear blood sugar problems (false negative) (Aust N Z J Obstet Gynaecol, 2014).
Others will fail the glucola despite normal blood sugar metabolism, but as a result of eating a healthy, lower-carb diet (false positive). I described the pros and cons of different testing methods in this post (and my own personal experience of failing the 50-gram glucola screen).
Myth #5: I’m Thin. I Can’t Possibly Have Gestational Diabetes!
Screening for gestational diabetes might seem like another unnecessary test, especially if you’re otherwise healthy, but that doesn’t mean you’re in the clear. Some studies have shown up to 50% of women with gestational diabetes don’t have any of the classic risk factors, like being overweight prior to becoming pregnant or a family history of diabetes.
While the screening tests aren’t perfect (see above point), it’s still worth being proactive given all that we know about mildly elevated blood sugar levels and risks to your baby. Even if you’re not interested in the glucose drink, at the very least, using a glucometer to measure your blood sugar levels for a few weeks while you eat your usual diet teaches you a TON about food and your body. And if you’re reading this in early pregnancy, ask to have an A1c added to your blood work.
Myth #6: Diet Doesn’t Matter or Change the Risk for Gestational Diabetes
Eh, sort of. Sometimes gestational diabetes is out of your control. And sometimes there are things you can do modify these risks. If you already have a positive diagnosis, do not beat yourself up. You can’t rewind the clock to lose weight preconception or change your family medical history and the important thing is to focus on what’s in your control: how you eat and care for your body (and baby) NOW.
With that disclaimer out of the way, studies are showing that what you eat can lessen the risk of gestational diabetes, at least for some women.
Your pancreas, the organ that produces insulin, undergoes dramatic changes in pregnancy as it prepares to pump out at least triple the amount of insulin (this is to overcome the innate insulin resistance of late pregnancy and to keep your blood sugar in that nice 20% lower than usual zone). In order to do this, the pancreas needs enough of certain amino acids, suggesting that inadequate protein consumption during the first trimester is a risk factor for gestational diabetes. (Nat Med. 2010)
Another study found higher rates of gestational diabetes among women who ate more cereal, cookies, pastries, and drank juice, while lower rates were found in women who regularly ate nuts (Clinical Nutrition, 2016). Simply eating more than your body needs is a risk factor, given that excess weight gain, especially in the first trimester, ups the odds that you’ll get gestational diabetes. (Obstet Gynecol, 2011) Overconsumption of high-glycemic carbohydrates, in particular, is consistently linked to excess weight gain.
“Altering the type of carbohydrate eaten (high- v. low-glycaemic sources) changes postprandial glucose and insulin responses in both pregnant and non-pregnant women, and a consistent change in the type of carbohydrate eaten during pregnancy influences both the rate of feto–placental growth and maternal weight gain. Eating primarily high-glycaemic carbohydrate results in feto–placental overgrowth and excessive maternal weight gain, while intake of low- glycaemic carbohydrate produces infants with birth weights between the 25th and the 50th percentile and normal maternal weight gain.” (Proceedings of the Nutrition Society, 2002)
This might surprise you, but excessive fruit intake in pregnancy is linked to higher odds of gestational diabetes, especially high glycemic fruit (more is not always better when it comes to fruit).
“An increase in total fruit consumption during the second trimester was associated with an elevated likelihood of GDM (highest vs. lowest quartile: crude OR, 3.20; 95% CI, 1.83 to 5.60). After adjustment for age, education, occupation, income level, pre-pregnancy BMI, gestational weight gain, family history of diabetes, smoking status and alcohol use in Model 1, a significantly higher likelihood of GDM was still observed in the third and fourth quartiles for total fruit consumption (OR 2.81; 95% CI 1.47 to 5.36; OR 3.47; 95% CI 1.78 to 6.36, respectively).”
(Scientific Reviews, 2017)
Myth #7: All Women with Gestational Diabetes Will Have Big Babies
Not so fast… One of the big fears associated with gestational diabetes is the risk of having a large baby (also called macrosomia). Statistically it’s true. As a whole, we see more macrosomic babies among women with gestational diabetes. However you don’t have to be a statistic. The chances of having a large baby correlates very strongly to blood sugar control during pregnancy. (Int J Gynaecol Obstet. 2002)
So if you know what to do to keep your blood sugar under control, your risk of having a big baby goes way, way, way down. And if your blood sugar stays at pretty much normal levels, you are at no higher risk than a women without an “official” gestational diabetes (and probably a way lower risk than someone who had a false negative on their glucose screening and is eating whatever they want without any consideration for their blood sugar).
I have yet to have a participant in my online Real Food for Gestational Diabetes Course have a macrosomic baby. Take that, statistics.
Myth #8: Cut Back on Carbohydrates, BUT Not Less Than 175g of Carbohydrates/Day
The conventional nutrition advice for gestational diabetes is mind-numbingly nonsensical. You’re given the diagnosis of GD, aka “carbohydrate intolerance,” yet told to eat a bunch of carbohydrates. You fail a 50 or 75 gram glucose tolerance test, yet are told to eat 45-60 grams of carbohydrates (which turn into glucose in your body) at almost EVERY MEAL. It’s no wonder roughly 40% of women will require insulin and/or medication to lower their blood sugar when they’re consistently filling up their carbohydrate-intolerant body with lots of carbohydrates.
Perhaps not-so-shocking is that researchers have shown that eating a lower-glycemic diet reduces the chance a women will require insulin by HALF. (Diabetes Care, 2009) It’s common sense, friends.
Unfortunately, there’s oodles of misinformation low-carb diets. Women are warned not to eat low-carb because they might go into ketosis (even though virtually every pregnant woman is in and out of ketosis on a regular basis). Plus, there’s entirely no acknowledgement that ketosis can exist outside of diabetic ketoacidosis. Sadly, few healthcare professionals have fully investigated the details and continue to fear-monger based on false information.
I’m one of the few that has done the research and I’m the first dietitian to scientifically defend the safety (and benefits) of a lower-carbohydrate diet to manage gestational diabetes (see Chapter 11 of my book, Real Food for Gestational Diabetes if you want the research-y breakdown).
I’ve spoken at numerous conferences on the controversies surrounding low carb diets and ketosis during pregnancy. If you’re a clinician, I have a web-based training on gestational diabetes which not only covers blood sugar management using my real food approach, but also dives deep into the research on low-carb diets, ketosis, and pregnancy as a whole. Get more info on it here.
Myth #9: You’ll Need Insulin No Matter What
That’s simply not true. The first step to managing your blood sugar is food and lifestyle tweaks, not insulin.
Now, if your healthcare provider is only familiar with conventional, high-carbohydrate diet therapy, they probably end up prescribing insulin or blood sugar lowering medication a lot. But, again, you do not automatically get put on insulin and you have the option to make more informed dietary choices to reduce your chances of needing it in the first place.
Don’t get me wrong, insulin can be an amazing tool, and, in some cases, it is needed. But, if your pancreas is still producing insulin (it’s usually producing a LOT during pregnancy) and if you can make changes to lessen your blood sugar spikes (easing the insulin demand from your already over-worked pancreas) and reduce your insulin resistance (like changing your diet and moving your body more, etc), your chances of needing insulin shots goes down.
By the way, if high fasting blood sugar is what you’re struggling with, I have an entire advanced training on lowering fasting blood sugar naturally in my online Real Food for Gestational Diabetes Course.
—
Whew, that was a lot and I feel like I’m just getting started. There are so, so many gestational diabetes myths and I’m passionate about helping you sort through the nonsense, the science, (and the non-science?).
I’d love to hear your thoughts on this post in the comments below. Which myth surprised you the most? Are there any other things you’ve heard about gestational diabetes that you’re not sure about? Leave me a note in the comments below, so I can address them in a future blog post.
Until next week,
Lily
PS – If you’re a clinician/healthcare professional working with mamas with gestational diabetes, I have a continuing education training just for you. This webinar goes into the science of gestational diabetes, why blood sugar management is so crucial, the safety & controversy of low-carb diets during pregnancy, tips for managing fasting blood sugar naturally, and much, much more. I share clinical pearls in this training that are not available anywhere else. Get the details here.
PS – If you were just diagnosed with gestational diabetes and want to learn how to manage it with real food (and lessen your chances of requiring insulin), be sure to check out my FREE video series on the topic. You’ll get 3 in-depth videos + a guide to managing your blood sugar at absolutely no cost to you. Sign up HERE.



Great info Lily! I am in shock that some health care professionals don’t believe it is a true diagnosis. Knowledge is power to help reduce complications of GDM.
“Knowledge is power” is a continual mantra in my practice.
Thank you so, so much for writing this, and for all the work you do. Your book was the only thing that made any sense when I had gestational diabetes. I noticed I couldn’t handle more than 30g of carbs in a meal. More than that, and my blood sugar would be elevated, which is dangerous to my baby. But then the nurse or the dietitian would tell me if I didn’t eat more, I was starving my baby of carbs. How does that make any sense?! The baby gets his carbs from my blood stream!
I also had no risk factors other than family history (115 pounds pre-pregnancy), was allowed to go into labor on my own at 41 weeks, and had a 100% drug free (I wasn’t even hooked up to an IV), vaginal birth to an 8lb baby. I listened to my gut and never needed insulin or medication. I was a myth-busting machine!
One thing I’d like to learn more about, is blood sugar during labor and immediately after birth. I was in labor for 24 hours. Between dinner Monday night and by son being born just after midnight on Wednesday, I didn’t consume anything except tiny sips of apple juice (my choice). I also threw up twice. But my blood sugar was steady the entire labor. However, as soon as he was born it shot up. I think it was 180-something right after birth and by the time I could stomach food again (after 36 hours without) it was at 220+. By the time I left the hospital it was back to normal. What processes were going on there?
Hi Chloe, Yes. That’s a story I’ve heard far too often and a big reason I wrote my book and created my online Real Food for Gestational Diabetes Course. Congratulations on a healthy pregnancy and natural birth!
That’s an interesting observation about your blood sugar post-birth. I’m afraid there’s really not much in the literature on trends in blood sugar in the immediate postpartum period (outside of women with type 1 diabetes). I’d guess that a blood sugar surge is possibly due to increased stress hormones and all the inflammation/immune response that follows birth. But, I’d definitely follow up with your provider and get your blood sugar tested after 6 weeks postpartum (which is recommended for anyone with GD).
I want to thank you. I was diagnosed gd and I wasn’t happy with the high carb diet my dietitian suggested me, my glucose levels were out of control. I am also coeliac. After two weeks of this diet, I found your blog, bought your book and followed your principles, always under medical control. I had to use insuline only before going to bed to control the glucose during the night. My baby is born 2,955 kg and with perfect levels on glucose test! ? The diabetologist was very surprised. I really don’t understand why they keep suggesting so high carb diet for gd.
Well done!
Interesting. I was also prescribed a high carb diet. When I was in the nutrition class, I was shocked at how much carbs they wanted me to eat since I was not much of a carbs eater (breads, rice, starches of other sorts) outside of fruit and fruit juice ( I am a runner, so that’s how I carbload). My glucose readings were in the 150s one hour after eating. They told me I would need to be on insulin, so I told them I was going back to my regular diet. Since then, my blood sugar levels have been well within range, including my fasting levels. I pretty much don’t take the nutritionist’s advice anymore, especially when she recommended eating a McDonald’s breakfast biscuit for breakfast. So strange.
Lily thank you! Your information is invaluable to practitioners! I am an RD working in outpatient pediatrics and am starting to move that into including more prenatal/early childhood. I have 2 quetsions:
1. What if I suspect a mama has that false + glucose test? She has been following a low carb diet for a few years now, never has BG issues, super active and then “failed” the test, and not by a large margin, by the way-it was close to borderline. I have been so perplexed by this and then read this post about the potential for false positive! Wow! What could I suggest the OB test in order to see if it was false?
2. Have you ever considered a series of trainings for RDs?? We need this info and it’s just so hard to get!!
Thanks!
Megan Wroe, MS, RD, CLEC
Hi Megan,
Regarding your questions, I think it depends. There’s no harm in testing blood sugar and having reassurance that her numbers are normal. Her OB should understand that it’s not the label that matters, per se, but the overall blood sugar control. Some OBs will just mark the existing results as a false positive (not GDM) if their blood sugar numbers are truly following normal pregnancy blood sugar patterns (like I cited in this article). But, if she’s really keen to have an official un-diagnosis, she could carb load for a week or more prior to a repeat OGTT and hope for the best.
And to question 2, yes. Absolutely. I have plans to host online trainings/webinars as well as speak at more conferences. 😉
The main blood sugar reading I’m having the most problems with is my morning fasting reading. All others appear to be directly related to what I eat. Can you offer me any insight into what’s at play with the fasting sugar reading? My HgA1c was mid-4’s first trimester and 5.7 in third trimester. Not too crazy… I’m planning on buying your book, but am unable to take your course. Will this be covered in your book? Or can you refer me to any other resources? Thank you so much for your time!
Hi Katie, Yes, I do address fasting blood sugar in my book, though the fasting blood sugar training in my course is far more in-depth.
I’d definitely be in touch with your healthcare providers about the rise in A1c. It usually stays the same or goes down as pregnancy progresses, so a jump like that is actually pretty significant.
Hi Lily, Thank you as always for your words of wisdom. I would love to hear more about the false positive scenario. I failed the glucola tests miserably but had none of the classical GD symptoms during my pregnancy, had already been following your diet recommendations, and my blood sugar was never above 110 when I tested it. I would love to see more research or information about this “false positive” scenario.
This post will help explain the false positive situation.
Thank you for this! When I was pregnant with my first child back in the 80’s no one even thought of this. I gained a lot of weight, lost most of it after giving birth but couldn’t shift it all, gained and kept a bit more weight on after two more babies. Tried everything to lose it and by the time I was 50 I weighed 220 lbs . My joints were inflamed, I could hardly walk, my blood pressure was up, I felt awful. In desperation I tried the much vilified Atkins diet….and lost 70 lbs in less than a year, my health issues cleared up….I wish someone had given me the advice you have here, I would have been able to manage my insulin resistance and not have spent half my life feeling like an overweight failure! I now maintain a healthy weight by keeping to a ketogenic diet!
I’m trying to make up for decades of misinformation! Glad you’ve found what works for you, Lorraine. That’s a truly impressive transformation and testament to the benefits of low-carb. 😉
Thank you so much for all of this great information!
I have a question that i haven’t been able to find any information on: I had read that during pregnancy there are hormonal shifts (28-34 weeks being a big one) that can interfere with insulin response and cause higher readings in GD pregnancies. Does this hormonal shift affect non GD pregnancies as well, perhaps to a lesser degree (slight rise from baseline blood sugars)?
Yep, that’s physiological insulin resistance that happens in every pregnancy, however the body is able to compensate for it and keep blood sugar under control in women who don’t have diabetes (or pre-exisitng insulin resistance/prediabetes coming into pregnancy).
So you’re suggesting that if your body isn’t able to compensate, it’s because you had some form of pre-pregnancy insulin resistance/prediabetes? Where is the literature to back this up?
Not always, but this is one of the presentations of gestational diabetes, often confirmed with A1c readings in the first trimester in the prediabetic range (a surrogate marker of insulin resistance prior to pregnancy) or other lab markers of insulin resistance taken in early pregnancy or pre-pregnancy. A few studies to get your research started…
Amaefule, Chiamaka Esther, et al. “The accuracy of haemoglobin A1c as a screening and diagnostic test for gestational diabetes: a systematic review and meta-analysis of test accuracy studies.” Current Opinion in Obstetrics and Gynecology 32.5 (2020): 322-334.
Boe, Brendan, et al. “Universal early pregnancy glycosylated hemoglobin A1c as an adjunct to Carpenter-Coustan screening: an observational cohort study.” American Journal of Obstetrics & Gynecology MFM 1.1 (2019): 24-32.
Arbib, Nissim, et al. “First trimester glycosylated hemoglobin as a predictor of gestational diabetes mellitus.” International Journal of Gynecology & Obstetrics 145.2 (2019): 158-163.
Bender, Whitney, et al. “Universal HbA1c screening and gestational diabetes: a comparison with clinical risk factors.” The Journal of Maternal-Fetal & Neonatal Medicine (2021): 1-7.
Benhalima, Katrien, et al. “Characteristics and pregnancy outcomes across gestational diabetes mellitus subtypes based on insulin resistance.” Diabetologia 62.11 (2019): 2118-2128.
I’m so glad my midwife shared this post with me. It’s seriously the most eye-opening, yet well-written post I’ve read on gestational diabetes. Thank you so much for sharing your expertise and so much research. – Ann
PS – I’m buying your book ASAP!
Thanks so much, Ann. Glad it was helpful and I appreciate your support.
Hi,
Just curious, the 20% lower values for mean blood glucose, were they collected along the pregnancy or during a specific period (namely the end of the 2nd trimester through the 3rd)? I think it would be really useful to differenciate these as the behaviour of blood sugar is completely differente, as you state in your text, between 1st and subsequent trimesters.
It would be helpful for all women to know what values to target during the 3rd trimester, instead of just being happy about being below the limit, and giving their babies the best chance possible.
Thanks.
Good question. That study compiled patterns of blood sugar in healthy pregnant women (non-diabetic, healthy weight) from 11 studies. Average gestational week was 33.8 +/- 2.3 weeks, so third trimester. Pregnancy-induced insulin resistance doesn’t kick in until later in pregnancy and even still, the natural and preferred blood sugar levels in late pregnancy are surprisingly low. Given this finding, the authors suggest lower blood sugar targets for gestational diabetes.
Would you mind sharing the bibliographic info for that study. I’d really like to read it!
Hernandez, Teri L., et al. “Patterns of Glycemia in Normal Pregnancy: Should the current therapeutic targets be challenged?.” Diabetes care 34.7 (2011): 1660-1668.
Hi! I had a similar question. Is there a way for your to provide a link to the full meta analysis and research you referenced? I so appreciate you using evidenced based research, but am curious about sample sizes, co-occurring conditions, the impact of stress and illness on measures temporarily, etc. Thanks!
I’m so grateful for your book. I have a nasty family history of Type II diabetes. I feared it and workout like crazy, but my eating was a piece of the puzzle I wanted to turn a blind eye to. When I was diagnosed with GD I purchased your book right away. I actually lost weight and felt better than ever, easier than ever before. I have a medical team that really forces the high carb/ketosis is horrible. I know your plan was working. I do hope that more medical professionals are trained and this becomes common knowledge. I’m 37 weeks and looking to a healthy estimated 7lb baby
Way to go, Charlotte!
By the way, many people gift my book to their doctors. The Czech Republic changed their official gestational diabetes guidelines and dropped the minimum carbohydrate recommendation based on the research I review in my book, so there’s hope. 😉
So my question has to do with after giving birth? I’m told I will need more carbs than I have been consuming with my gd diet (did better controlling with diet alone the first 2 times this time I’m on glyburide for fasting) when I found out I was pregnant I was in the middle of a keto lifestyle change to get in better shape I was doing well and would like to go back to it once the baby is born as my weight loss didn’t stop but definitely slowed when I went back to consuming carbs. Can I go back to it and still produce enough milk for my baby?
I address breastfeeding nutrition and low carb in these interviews:
https://lilynicholsrdn.com/carbs-required-pregnancy/
https://lilynicholsrdn.com/real-talk-breastfeeding/
This. Is. Fantastic. I can’t thank you enough for this information. I am also passionate about the standard of care for diabetes (GD included). I wish more doctors were willing to learn about the benefits of this type of approach. I am not pregnant (yet) but my mother had GD when she was pregnant with me. I think this has had an effect on my ability to maintain my weight my whole life (as well as the outdated food pyramid growing up, being part of the “low fat” generation, etc.). I think my body is still confused! The last thing I want is to pass that on to my baby. I have been working to lower my weight BEFORE getting pregnant in hopes to avoid the issues so many end up with.
THANK YOU!
Thanks for writing this article! Third pregnancy, first with GD, so I’m learning a lot. I would add that doctors are not always or even often so quick to be as resistant to alternate approaches as some imply (not necessarily in this article, but some really blast conventional medicine sometimes). Due to moves, I have used three different OB groups–one per pregnancy-and they do not use the sort of rigid, unfeeling, habit based treatments that a lot of pregnancy articles claim. If you use an OB, talk to them. Don’t feel that your only option is a midwife, especially if a home birth is not what you want. There are scientific studies that support all kinds of birthing and pregnancy philosophies, and the more I research, the harder it is to trust anyone due to the tendency to disregard research findings that don’t match personal philosophy. Somehow only those studies are tainted by [insert preferred big baddie here]. Find someone you trust who will birth your child and help you manage your pregnancy in good health, and accept that not everything will be perfect or in your control. And don’t fear using an OB–sometimes I wonder how much fear mongering against hospital births is just a form of advertising for competing midwife services. I have had wonderful hospital births with epidural and immediate, high quality care for tears as well as serious birth issues that arose during my “low risk” delivery. Glad I wasn’t only “minutes away” when seconds counted. Everything has a downside.
Sorry, just had to reply to the statements about midwives. I am not a midwife, nor do I think that all obstetricians are bad, but there is a history in this country of prejudice against midwives by the AMA, and individual physicians. So much so, that when obstetrics as a profession was being established (not too long ago), there were campaigns designed to portray midwives (many being immigrants and/or women of color) as dirty, superstitious and uneducated. I’ve personally heard obstetricians express some very insulting (and untrue) opinions about midwives. Yet, I also know some doctors who value midwifery and work closely with CNMs— and vice versa. Look at the UK model; it doesn’t need to be either/or.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2582410/
https://qz.com/1119699/how-racial-segregation-led-childbirth-in-america-to-be-over-medicalized/
https://www.lib.umich.edu/online-exhibits/exhibits/show/reproductive-justice/overview-whose-birthing/grand-midwives-versus-the-
https://pmj.bmj.com/content/78/919/311
https://midwiferytoday.com/web-article/history-midwifery-childbirth-america-time-line/
I absolutely agree with you that a hospital birth is the safest when every second counts (and not all of us that birth in hospitals want an epidural either, nor are they required, as the home birth crowd often alleges).
I also agree that much of the fear mongering about hospitals does come from the pro-midwife lobby. Regardless of the past, they are not some kind of “underdog” – they have lobby groups just as the drs do, and some states are even now covering midwife services with insurance.
To the commenter who replied to you, comparing home birth midwives in the US to European countries is apples and oranges. Other countries often have standzrdized training and education for midwives, they work within the health system, are trained nurses. US midwife training (or lack of) and licensing varies by state, with some states allowing literally anyone with no training to call herself a midwife, most are not trained nurses, and work outside of/against the system.
The only thing i would disagree with you about it that *most* drs are open to alternatives. In one of my previous pregnancies i had the most easy going dr who let me skip the glucola test and just test myself at home, no attitude whatsoever.
My insurance changed for this pregnancy, an I’m stuck with a dr who told me he would dismiss me as a patient if he could, gave me major attitude, and wants to refer me to a high risk dr, all for refusing the glucola and offering to do self tests instead. So it just depends on who you get, your insurance covers, and luck.
Thanks for this article. I was diagnosed GD with my first. Luckily/annoyingly my practice takes it very seriously… I was GD by 1… Three hour test I was 1 hr test high, two hour at the lowest number considered high and 3 hour all the way back down… And my fasting was typically low 70s. I ended up being induced at 39 and 6 days bc of practice liability rules, even though I was diet controled the whole time… Ended up with a prolasped cord and an emergency C… and my son was only 7lbs 3oz. I was wondering for my second go if you had any tips to have things go better… I feel like they took my son to early and my body didn’t respond to the induction drugs well. I would much rather be given the chance to go into labor on my own… Any thoughts for a more favorable outcome?
Pregnant women have so many hands in the pot due to everyone wanting what’s best, listening to yourself and listening to the Dr.’s, who are supposed to know what’s “best.” If your glucose and weight were under control and the baby was healthy, then you have every right to want to wait and see. It’s your body and your baby. Induction has a high risk for prolapse and C-sections especially in a woman who’s body is “unfavorable” (there are signs to look for and you should get a favorable conditions for labor number and likelihood for success). IMO liability is not a proper reason to just induce a person. There needs to be a legitimate medical reason to do so and do so under favorable conditions if at all possible. Patients have the right to refuse treatments and procedures (it’s in that booklet of patients’ rights that no one reads). I do not know your medical history or if the end result may have happened anyway, but I just wanted to let you know some of the facts. A more favorable outcome may be getting a different Dr. if possible. I cannot tell when this post was made, but much has changed in the way of labor policy in the past 5 years (today Jan.2019). I am an RN, passionate about women’s health, and I have seen both the good and the bad in L&D.
Thank you very much for this information. I am 6 weeks pregnant with my 3rd child. I had a GD diagnosis with my 2nd child and had always wondered if I ate a low carb diet from the beginning of my pregnancy if my risk of developing GD could be drastically reduced with subsequent pregnancies. I will be buying your book. Thanks for making this information available!
Megan
Lily, I am curious whether any research has been done regarding diet in first trimester and a Gestational Diabetes diagnosis? I have a healthy BMI and I generally eat well, but in both my pregnancies have suffered terribly from severe morning sickness in the first and second trimesters. My diet in the months prior to the GTT was very limited but incredibly carb heavy – I could only tolerate bread, potato and orange juice. Certainly no exercise either. In both my pregnancies I have failed the GTT only on my 2hr levels. I wondered whether there was any connection.
Hello,
Will you please add a list of references? I would love to look at these studies my self and your abbreviated footnotes don’t have quite enough information. Thank you!
Thank you for this post! I am 25 weeks pregnant; this is my first pregnancy and I have already 9 kgs in weight. I have been diagnosed with gestational diabetes after the 50mg glucose test (result: 179 mg%). How serious is my case? Can I still lower the blood sugar level if I eat healthy? How much do I have to worry about my baby’s health? I am actually freaking out!
I was just diagnosed with GD and freaked out. It’s been a few days and my blood sugars 1 hour post meal have been 80-100. I’ve definitely tweaked my diet and gone low carb. My doctor is recommending eating at least 200g of carbs/day. I’ve been eating closer to 100-140. My fasting glucose seems to be the real problem, usually between 95-105. This article definitely gave me more insight into the world of gestation diabetes. Thank you!
Hello! Thanks for all the great info! I’m see a dietitian next week bc i failed my 3 hour test. I failed the resting and my first blood drawl after drinking the glucose stuff. My 3rd was fine and my fourth one was only 50 and I almost passed out. Do you think my body over compensated for the earlier high one?
Great article! I was diagnosed with gestational diabetes just before my 3rd trimester. I was at a healthy prepregnancy weight(120lbs), but because of family history I took the glucose tolerance test at week 14 of gestation. I passed with flying colors, but when I retook the test at 28 weeks I failed both the 1 and 3 hour. There was a lot of misinformation out there, and I was so afraid of needing insulin, and even worst having a large/unhealthy baby. I’m happy to say that with simple dietary changes I gained 30lbs during my pregnancy, kept my blood sugar under control, and my baby was born at 40 weeks 3 days weighing 6 lbs 14 oz. I feel the GD diet helped me to quickly lose the pregnancy weight as well! I didn’t get stretch marks, and I lost 20 lbs within 2 weeks of giving birth. I attribute this to sticking to the diet.
Hi
i have gtt reading 4.68 10.3 8.3 my dr said i have gdm.then after 15days i have normal fasting pp glucose and hba1c. I am confused i have gdm or not?
I have gestational diabetes for the 2nd time and I told my doctor that lowering my carbs helped me out tremendously, but she argued with me about it stating that it wasn’t a good idea during pregnancy. I told her I wanted to avoid medication so I did a ton of research, but she was not interested in anything else I had to say. I went with my instincts the first time around and my daughter was a little under 7lbs when she was born and I went into labor naturally.
This was excellent information. I was keto prior to pregnancy. Now I stay low carb but have added back in the natural sugars from fruit. In the last few days I have been under 50 carbs a day. Does that influence the glucose test?
This is such great information. I was just diagnosed with gestational diabetes. The recommended carb load blew my mind! The 175/day carb load recommended by my doctor seemed nonsensical. I don’t actually know how I would eat that much food in a day. I’m not that hungry. The first day when I tried to be a good patient and eat the numbers the doc gave me my blood sugar was really high. Low carb has gotten my numbers into a sweet spot. Now I can keep eating low carb without guilt.
What a great article. So many of these are true for me. I was beating myself up thinking I’d done something wrong and realized quite quickly that I did nothing wrong, it is just one of those things. My babies were small, my one was born weighing 6 lbs 3 at 39 weeks and my daughter was 6 lbs 15 at 40+3 weeks. I was never put on insulin with either of them. There are so many misconceptions out there about GD so it’s very refreshing to read your article 🙂
My doctor told me that my GTT results have just touched the border line.. I am 25 weeks pregnant.. Doctor just asked me be on diet but haven’t suggested anything in specific.. Can you please advise of what foods can I add to my diet and how cautious am I supposed to be now to avoid further complications
I have been diagnosed with GD. I’m checking my blood sugar 4 times a day, and have been between 80 and 115 each time but 1 (and it was 77). im very conscious of what im eating and I wasn’t overweight before this pregnancy (my 3rd), and i havent gained weight beyond whats recommended. do you think it’s likely I had a false positive on my GD test? beyond continuing to choose foods carefully and exercise, i dont know what to do to make sure baby stays as healthy as possible. thanks for any insight!
Thanks so much Lily, you are one of the only people out there that is making sense to me right now. My after meal levels have been low and under control but my dietitian told me to eat MORE carbs because my High protein/Fat and Veggie diet was going to hurt the baby. Also this crazy idea that all Protein, Fat & Vegetables are ‘free foods’ and don’t count! Still working to get my Fasting level a bit further down and have tried to high protein/fat before bed and plenty of exercise but it hasn’t helped yet. Any advice on this would be great. Thanks again
Hi Lily,
Thanks for the information. I haven’t taken the test yet but have been eating low carb/sugar for anti-inflammatory purposes. Are you saying that eating this way puts me at a risk for a false positive on the test?
Thanks,
Nina
Hi Lily,
I’m so bummed I’m just coming across your information now into my 3rd trimester. I wish I had this as preventative medicine pre-prengancy! I bought both of your books for real food and GD. I was diagnosed with GD a few days ago. I do not ingest any processed sugars but do have a low carb 75-90g daily diet and I’m concerned I also have a false positive. I’ve been curving at home and all of my 1-2 hour postprandial readings are between 81 mg/dL and 104 mg/dL at the highest.
My fasting BG is between 90-95 mg/dL though, and I’m wondering if you would comment and even consider a blog on the potential of dawn phenomenon for non diabetic women- whether that can be related to pregnancy or not I’m not sure.
Thank you kindly,
Emmily
Hi! Do you have a shorter course specifically for lowering fasting blood glucose only?
Thanks for this Lily, great post! It adresses so many of the “fights” that I had with healthcare personell over the course of my 5ish months with gdm. I was arguing against meeting at least 2 or 3 of those myths every time… I love that you included sources, would be great to see more details on those (so I can go read them myself, super interested)
All research in this post is cited in full in the references section of my book, Real Food for Pregnancy.
Your care team might be interested in the continuing education webinar I teach on gestational diabetes nutrition. Worth mentioning it to them at the very least. This presentation is also fully referenced.
I am feeling really discouraged and ran across your article. I am 8 weeks pregnant and weigh 175 lbs. I have been working with a trainer and am down from 190. However I recently started tracking my sugars and my fasting glucose levels every morning are in the high 90-95 range. Basically I am realizing I am prediabetic and just didnt know until now. Now I am really concerned about how this pregnancy is going to go. I plan to get your book. Just needing reassurance that this pregnancy can still go ok if I keep diet and exercise as a priority.
Hello Lily, do you have any advice for unresolved hyperglycemia 4 months PP? I diet-managing my GD with a mostly plant-based without much provider interference, baby was born naturally and healthy. I’m not overweight nor do I have much family hx of diabetes (one grandmother). I live abroad and don’t feel I can count on good health advice here. So discouraged!
Hi Lily, I have a question regarding adaptive glucose sparing and pregnancy. I am 32 weeks pregnant and I have been on a low carb diet for many years with a fasting bgl generally around mid 5’s(mmol). I have read many times that as a result of adaptive glucose sparing this is quite typical in long time low carbers. I have an A1c of 4.4 as of last weekend. Naturally I failed the GTT and have been diagnosed with Gestaional diabetes but I’m unsure what to make of the high fasting bgls. Is it technically Gd if I had pre-existing high fasting levels with a low a1c? Should I ask for a fasting insulin count to be done or is it of no consequence? My concern is that if this isn’t typical pathological insulin resistance, is there the same risk to bub and I?
I actually did require insulin with my last GD pregnancy. Low-carb didn’t lower my fasting numbers at all. I still ran 100-110 every morning. The only thing that helped, and I know it sounds too simple to be right, was when my endocrinologist told me to just make sure I ate 7g of protein for every 15g of carbs.
I’m pregnant again, 8 weeks, and the OB’s plan is to start the slow-acting insulin right away at 10 weeks this time. Since I gained 25 lbs from insulin last time that have stuck around, after only 12 weeks on it, I’m sure Ill game 40-50 lbs this pregnancy.
I failed my 1 hour glucose test with my second child (a girl), but passed the 3 hour long one. She was born with blood sugar issues and had to be in the NICU for a week to make sure she could regulate her levels. The nurses that tended to me immediately after her birth said that if you fail the 1-hour test, you have gest. diabetes no matter what. Now I’m pregnant with my 3rd (a second girl) and just heard I failed the 1 hour test again. Does what they said have any truth to it? Is it worth taking the 3 hour long test, or should I just cut out most carbs from my diet for the rest of my pregnancy?
The 1 hour test is not diagnostic on its own, so it needs to be followed up with another (whether that’s the 3 hour test or another option is a personal decision). You may find the section on diagnostic tests for gestational diabetes enlightening in Ch 9 of Real Food for Pregnancy. Or see this interview I did on the Birthful Podcast.
Hello. It’s a really interesting article. But I’m still confused. My first pregnancy was big, my baby was born at 4.450kg via emergency c section. I had glucose test done while pregnant but was all ok. This time, second pregnancy is a big one too. Glucose test was normal. But all scans shows baby is on the bigger size. They asked me to do blood sugar test ( pricking the finger at 36 weeks). Within tree weeks,all look fine except 2 readings 5.3mmol( on empty stomach should be less than 5.3) and second and last reading an hour after meal 7.8 mmol( should be less that 7.8 mmol). Just 2 ” rised” reading.
They are not sure if I have gestational diabetes… My husband family had a big babies. I still eat sugar and blood test is within norm.
What should I think and do??
Xx
I was Dx with GD with my first child. I tested 5 times a day and my carb diet was 25 to 35 for meals and 15 for snacks. My fasting glucose was never over 75 and I even had a few in the 40’s. The Dr.s did explain the risks but most were not worried and supportive. One Dr. was aggressive and told me I would have a 10lb baby and be a bad mother! I delivered at 39 weeks to an APGAR of 9 with a 6lb 10oz baby. I was not allowed to eat during my labor either. My second child did not have a Dx of GD and he came at 40w 1 day with APAGAR of 9 and 7lbs 8oz. I am now 29 weeks pregnant with our 3rd and my 1hr came back with the Dr’s wanting the 3hr. However, my 1hr was after 3 days of gastroenteritis and 3 days of essentially the brat diet because that was all I could stomach on top of losing 5lbs. I was so sick, my husband had to stay home to take care of me. I had 1 day of a “normal” diet and activity before my test. I am refusing the 3hr for many reasons. I am a healthy eater; I don’t binge and only eat when I’m hungry. I only drink water and even before I was pregnant, I only drank water. I am an RN and a huge supporter of proper nutrition and nutrition education. I just wanted to add my stats to the mix and also to say how different it is to have a baby without the RN title and then have 2 with it.
Hello, I just stumbled across your blog and I just purchased your book. I am 32 weeks pregnant and passed the 1 hr glucose screening at 26 weeks. I just had an ultrasound that showed the babies stomach is alarmingly large and they suspect I have GD, despite having passed the 1 hour test. I am set to take the three hour this in two days. I suspect, due to previous bloodwork, I passed the one hour because it is not fasting and will fail part one of the 3 hr test (when they check your sugar prior to drinking the drink) the fasting part. I have two questions:
1. Since finding this info out 3 days ago I have put myself on a keto diet, is that smart or not smart in terms of failing the 3 hr test?
2. Is there a real fear of ketosis in eating low/no carb and sugar? does your book discuss this? Thank you.
This is addressed in both of my books, but in greater detail in Real Food for Gestational Diabetes. The whole last chapter is about the controversies and research surrounding low carbohydrate diets and ketosis in pregnancy. xoxo
Hi, gdm doesn’t always shows a risk for type 2. I had 3 gdm pregnancies, was diagnosed with prediabetes in spite of low bmi, healthy diet, plenty of exercise and no family history of t2. But with a family history of t1. Fast forward, 4 years after my last pregnancy I was diagnosed with type 1 diabetes. No doubt. Low c peptid and plenty of antibodies.. 10 pct of women with gdm will develop t1 not t2. T1 will often develop slowly in adults and I’ve low carbed since first pregnancy…
Thanks for sharing your journey and highlighting the importance of ruling out type 1 diabetes. It’s far more rare than developing type 2 diabetes, but it does happen.
I am now in my 3rd pregnancy with GD and have had great success with diet control, specifically low carb. I am always perplexed at the medical world’s approach to medicating something that can be controlled and mediated through diet. Nevertheless, ketones seems to be something you deal with in low carb diets, making GD a virtual tight rope for me. I’ve always been told that ketones (while admittedly not completely proven) can be harmful to the baby. I’ve gotten scolded by doctors (OB’s) when I have had ketones in my urine. So, in addition to eating low carb, nutritious, whole foods, I have to be very careful to ensure that I also eat often enough. All that to say, I’m really interested in your research about ketosis in pregnancy. I think I’ll be checking out your book.
Hi Lily,
Thank you for all the useful information. I was diagnosed at 28 weeks and purchased your book immediately after and it has helped me considerably. I have been able to control my blood sugar numbers with my diet and doing some walking. However, I woke up this morning with a high fasting number out of nowhere and my numbers have trended high all day today. I am not sure what changed over night and am looking for some insight here. I will be 35 weeks tomorrow.
Regards,
MG
Hi, Lily-
I just had my second daughter and am a bit confused. For both pregnancies, I had diet-controlled GD; however, both girls were large and a bit early (8 lb 15 oz and 9 lb 4 oz). I am very perplexed because I followed a strict low-carb diet for both pregnancies and my doctors were pleased with my low blood sugar readings. For this last pregnancy, I began checking my sugars early on and adjusted my diet. My fasting numbers were typically below 80 and my 1-hour post-meal were almost always below 95. I was very careful with what I ate, but she still had was 9 lb 4 oz 2 weeks early and spent 2 weeks in the NICU! I’m beating myself up because I have no idea what I could have done differently. I would love to eventually have another child, but am afraid of failing again, despite my strict diet and efforts. Have you had any clients with this issue before? I read somewhere that if you don’t eat enough carbs then your body starts converting the fat and protein you eat to glucose. Is this possible?? Thanks for your help!
This was great! I’m 38 weeks and have been entirely diet controlled with a low-carb regimen. I was actually underweight until around 6 mos due to lack of appetite in the first trimester. Can being underweight up your risk for GD? Also, the lack of protein in the first trimester finding is super interesting. I couldn’t stomach protein then and wonder if that played a part.
This is so interesting!! I so wish I had known about these books before my last pregnancy! I really wasn’t sure what my carb intake should be, I usually do low carb diet similar to your plan, but since my goal obviously wasn’t weight loss, I ate more carbs than I usually would, I started out about 107 lbs, and gained 37 lbs. I wasn’t diagnosed GD but I did have a 8 lb 10 oz baby at 39 weeks, actually induced due to high blood pressure, close to pre-e. This was my second pregnancy and it was a lot harder, I had horrible middle of the night insomnia both pregnancies, but my first I was able to sleep when I could and got more excercise. Either way I’m thankful my baby is healthy, although big! If I ever have more at least I could be more confident in my diet and lifestyle choices!
Thank you for sharing such useful information. I have a question to ask.
Is it true, If the mother is suffering from Gestational diabetes during pregnancy are there any chances that the husband may suffer the same because they share the same diet?
I read this on https://www.myhealthyclick.com/diabetes-during-pregnancy-increases-type-1-and-type-2-diabetes-risks-in-family/
I am glad to know about these myths. Thanks for sharing.
I am diagnosed (in the border) with gestational diabetes in the first trimester.Right now i am measuring my capillary blood glucose level only in fasting and the values are normal but when i tried to measure after 1 hour meal,values are higher (160mg/dL).Now i am in 38 week of pregnancy.can you please suggest or comment what should i do?Is it ok if only the fasting glucose is normal?
Please give your suggestions
Thankyou
Ask your doctor, but that is definitely a higher number for 1hr post than my doctor wants me to have, and I’m surprised they have you only checking your fasting numbers.
My diet and exercise have always been good, recently diagnosed with GDM and am getting the ‘carb increase’ talk constantly which is frustrating because I still include lots of legumes, vegetables, quinoa etc in my cooking just not ‘traditional’ types of carbs or as many as they would like. My BGL are fine throughout the day but my fasting levels are high (5.0, 5.2, 5.4). How can I avoid taking insulin if I’m already doing the diet and exercise (and was doing pre-pregnancy). P.S 16 Protaphane seems to have made the most minute difference to fasting levels (4.4, 4.7).
I’d undiagnosed diabetes for 1st 9 weeks of pregnancy. at 9th week my HBA1C was 9.5. Now with diet and insulin my sugar level have almost come to normal. I’m in my 12th week now. What are my chances to expect a healthy baby.
Thanks so much Lily! I was diagnosed with GD but it seems to have completely gone away at week 35 of pregnancy.
Is that possible? My sugars are less than 110 no matter what I eat!
i have a question.
Why do we test accept blood glucose for pregnancy at 28 weeks?
thanks.
what are the preventions of diabetes?
Hello! I really liked your article. I read it while doing my 3h glucose test. I blessedly passed, but I feel like my numbers are borderline and I’ve been a big slug this pregnancy. I’m curious if it’s possible to follow your guidelines if I don’t have a glucometer. I just watched your first video and you said it was absolutely necessary, but I would think they’d be helpful?
Hi Lily,
I had gd with my second pregnancy dx at 28 weeks. It was diet controlled but my fasting number was always around 90. After pregnancy I passed the glucose test but my fasting number is always on the higher side on my annual blood tests (97). Considering this, is it a given I would end up having gd in my next pregnancy? Also is it true that with every gd pregnancy the gd starts earlier and is harder to control? And do the chances of the diabetes not going away after delivery increase with every gd pregnancy?
Maria
thank you for sharing this great article , please suggest meals during pregnancy that maintain the sugar level?
How do you justify giving a diagnosis of gestational diabetes to a pregnant woman who is otherwise completely healthy, not gaining excess weight, is “measuring small” to the point of being referred to a perinatologist to check for IUGR, and only missed passing the 3 hour test by one point? That is a margin of error, and in this case, I 100% believe did more harm than good. Maternal weight before pregnancy was 119 lbs and due to restricting carbohydrates, only gained 17 lbs. The baby was born 11 days early (yes, early!) and under 6 lbs, so tiny and early, exactly the opposite of what is normally expected of GD babies, which is late and large. What is the likelihood that the baby was early because it was basically starving in the womb. Why is the medical community not even considering that perhaps there needs to be a type 1 and type 2 for GD, like there is for normal diabetes? One type for the typical GD patient, basically (not to mince words) women who are overweight and unhealthy. And another type for otherwise healthy women, who may develop it because their body knows what it needs and is trying to increase the size of the baby to a healthy weight.
Love the info! It makes so much sense. I do have a question though. I am controlling my GD pretty well with my diet, but I am not following my dietitians recommendations of 175 carbs/day. If I did that I would definitely be put on insulin. My question is this: Will my low carb intake keep my baby from gaining the proper weight to be healthy? Currently she is right on target, but I am consistently under 50 carbs/day. Thank you so much!
Thank you! I feel like I have read every possible online source of info on gestational diabetes online trying to inform myself about diet controlled solutions. Low-carb has been relatively successful for me after a diagnosis about 4 weeks ago, but I am still very much in a trial and error phase, especially with my fasting numbers. Finally, after reading this, I feel like I have found a logical and comprehensive resource for information. Again, thank you!
What a great article! I’ve had gestational diabetes with both of my pregnancies. Was prescribed metformin during my 1st pregnancy for fasting numbers that were in the high 90s, I decided to skip the recommended bedtime snack of 15 grams of carbs and it naturally brought down my fasting numbers into the 80s. When I told my doctor this, her exact words were “but you need that snack”! The lack of education and research regarding gd is just appalling. During my second pregnancy I followed a low carb diet and very rarely had any readings over the recommended amounts and I found it so much easier to plan meals and manage my sugars versus the 150-175 carbs that’s typically recommended. Both babies born healthy weighing 7 lbs 6 oz and 8 lbs 3 oz.
Articles like this are very much needed, thank you for the research and sharing.
Thank you so much for writing this blog and the book! I downloaded the book right away and started following your recommendations on meal plans, meal plate. I am trying not to reduce my carb hugely as i have always been on generally high carb diet, and i am not sure if completely switching to drastic low carb in the final trimester is the best thing to do. However, overall i have surely reduced my carb compared to earlier intake and also spaced out the same, taking smaller portions along with protein/fat. This has helped me a lot! And I can see the effect in a day. I am hoping this routine will work throughout this pregnancy, will see how my body react in later days. This is my 2nd pregnancy, and 1st time i was diagnosed with GD a week ago.
Thank you Lily for Leading the charge! It is so frustrating that so many health care providers in OB still follow the “old school” recommendations. My clients have great success following a real food, lower carb, low-glycemic plan but have to battle with their stubborn health care providers. We need a revolution to get rid of the old school GDM “diet”
What is maximus level of ketones un Blood in pregnant?
Hi. I was diagnosed with GD a few days ago. I failed the 3-hour glucose test – only my fasting blood sugar was below the thresholds. I felt very sick after drinking the glucose drink and for most of the day.
I still haven’t met with the nutritionist. However, I have been monitoring my blood sugar for a few days now and my levels are very normal. I’m well below the 140mg/dl 1-hour after eating ( my levels are between 95-120mg/dl). How is this possible? Could it be that the test is just too much sugar for me, but I can handle normal amounts? Could it have been a false positive? Any advice?
Hello, thank you for writing this myth-busting article. I’m actually looking for concrete information on rapid sugars vs long sugars. I’m in France, and was diagnosed with GD at 26 weeks. They have advised me to check my levels 6x/day, once before, and again 2 hours after each meal. The guidelines here are a meal should be 1/4 protein, 1/4 carbs (grains, breads, potatoes) and 1/2 RAW veggies. And if I want a piece of fruit, I have to eat it with a yogurt or cheese, something milk-based. They also said I could have a sugary treat once every two weeks.
Well, it’s the middle of winter, and eating half a plate of raw veggies is nonsense. It’s also holidays, and I love baking and have been enjoying (sparingly) some treats. My levels are very rarely high, and I’ve gained very little weight, and baby is not considered large at all.
What I’m wondering though, is if I have a rapid sugar treat after a meal, and 2 hours later the blood sugar is back down to normal, am I missing the dangerous spike which could harm my baby?
Thank you so much for putting all this information out here. I love your book! It is just hard for me to find some clarification/confirmation in any research that it is okay to have large ketones (8.0). I can’t seem to get them down. I drink lots of water and eat plenty of calories, healthy fat, proteins and around 100 grams of carbs a day. Is this something I should be worried about? Or at least, is this something you have seen before?
I found the answer! I could not understand it, because my sugar levels were always well within range and I was not even eating as low carb as recommended for keto diets to go into ketosis. I found it on a keto website that drinking water was not enough. You need electrolytes too. I got a couple bottles of electrolyte water, and the ketones disappeared immediately! Not even trace amounts left. I hope this helps someone else, if they ever come into this problem. It was causing me so much stress to see my ketones so high with no answers.
Hi Lilly,
My Doctor has told me my baby is measuring 3 weeks ahead iv done everything to keep my blood sugar managed but cannot get my fasting number to be controlled especially with insulin. I have 40 days to go. Can i reverse anything within this time frame for my baby. Im getting so worried.
I was t2d prior to getting pregnant. I was doing a keto-carnivore diet to help regulate blood sugar but still need a lot of work. Can you explain why I would take insulin if I already have too much? If my OB wants me to take insulin, do I have to?
Great info! I was very skinny before my pregnancy and ate healthy and still ended up with gestational diabetes. Of course I was told to eat carbs but noticed my sugar is still spiking. I went on a very low carb diet and did not need insulin. Had no issues with high sugar during labor and my baby did not have low blood sugar after birth. My biggest problem was controlling my morning sugar so I made sure to have protein at night and a tablespoon of apple cider vinegar. My doctor was not worried about ketosis and was happy I didn’t need insulin.
Hi Lily! My midwife pointed me in your direction after I got the results from my Glucose Screen last week at 28 weeks. I’m incredibly interested in everything you have to share! I have been exploring your sight, reading your blog, and have signed up for the video series. I’m going to purchase your book and do my best to control this with diet and exercise. I wish I had know to test much sooner. I’m hoping I can act fast and take control during the last trimester. Thank you for sharing your knowledge! It’s greatly appreciated in a world so controlled my medicine and fear.
What should be the range of sugar levels in gestational diabetes?
This is covered in my free video series on gestational diabetes (and in my book, Real Food for Gestational Diabetes). More information on both here: https://realfoodforgd.com/
I believed that one GD diagnosis meant I’d have GD for my next pregnancy as well. When I got my diagnosis at 30 weeks I dove into the deep end looking into the foods I ate under the assumption they were healthy & discovered so many options marketed as healthier had more sugar or carbs than “regular” foods. I completely changed my diet those last 10 weeks to include balanced, low carb, healthy fat & protein meals. I delivered a perfect 8 lb boy without any intervention (smaller than my husband & brother, who were born without GD being present & were both 9 lbs). Both of our levels were healthy after birth. Knowing that we were both at a higher risk for developing type 2 I continued our focus with my new information of what is truly a healthy diet. When I became pregnant again 2 years later I expected another GD diagnosis. I purchased your book, monitored levels & when it came time to test I was in utter shock at how fantastic my glucose levels were. I called to confirm they didn’t get them confused with another patient. I had a 6 lb 14 oz baby girl in April. I like to follow your page now because it truly seems like the best “diet” to follow regardless of being diabetic or pregnant.
Im glad to have read this. I am 20 weeks pregnant and didnt want to have the Glucola test. I cant quite get from your article if you recommend it or not. Also when people ‘test their blood sugar’ after they eat and stuff how are they doing this? Does it require the prick to the finger? I have a phobia of needles and avoid them at all costs so really need help determining what I absolutely need to do for my baby. Thankyou
Hi, I’m 30 weeks pregnant and was diagnosed with gestacional diabetes on week 25. Since then I’ve been put on a diet where I’m eating much more carbs than before. As my glucose levels on blood were not coming down, I’m now 3 weeks into insulin shots, first 6U/day, now 10U/day. I feel like I’m eating too much carbs and the carbs resistance will keep going up but the doctor says I need them for the baby. I was wondering if I could somehow try to change my diet to see if my sugar levels come down while taking insuline? Do you think that would cause me any problems? I fear that the levels can go down to very low and get adverse reactions. Thanks!
I’ve been checking my levels at home this pregnancy in advance of the test so my Dr takes me seriously when I decline the drink, I’ve been noticing my fasting blood sugar can be higher than usual but goes back to good range after meals. I haven’t been tracking food with it but my last fast was 6.9mmol/l (124mg/dl?), highest it’s ever been and I’d had a pretty high carb snack before bed the night before. A fast in this range has happened 3 times in the last two weeks..other 2 were 6.1 and 6.2 — it seems good and normal every other day so far. Is this a sign of GD?
I was diagnosed as a type 2 diabetic almost a year ago in my late 30s. My hba1c was 13.3% on diagnosis. I started out on 2 metformin 500mg a day with the advice that I’d need to increase my dose in the coming months and sent on my way to muddle through this thing on my own with the advice to lose weight, eat low gi carbs and excercise. Started to do that but researched more and realised that carbs weren’t my friend and that minimal carbs were a better option for me.
Within 6 weeks of diagnosis and going low carb, I’d halved my hba1c to 7.6%. Six weeks after that my next hba1c was 5.6% and its maintained that for almost a year now. We were about to start to try and conceive and I asked my doctor for a referral to a pregnancy and diabetes counseling program run at my local hospital that has a specialist maternity unit that provide care from preconception through to the birth of your baby. They were all confused as to why I was there because they just took my hba1c of 5.6% at face value and when I told them my history and that I’d gone low carb, they dismissed it as my normal range hba1c solely being the result of excercise and weightloss. As much as that helped I still think that low carb was the biggest reason for my readings.
They basically gave me the go ahead to safely start to try for a baby but told me low carb led to poor outcomes for pregnancy but wanted me to eat between 30 -45g of low GI carbs 6 times a day when pregnant. I have a bgl tester and anything now as a non pregnant person that is over 20g of carbs in a sitting irrespective of whether its low GI or not, spikes me into high numbers. It seems so silly to me that they tell me to eat so many carbs but expect me to have even tighter blood glucose control than I have now! They kind of scared me that being low carb during pregnancy will cause development issues with my baby but because they cant really ethically do studies on this with pregnant women, they base their evidence on a study done in mice and one on the keto diet in people using it to manage epilepsy. The people in the epilepsy study were also taking strong meds to manage their illness but I find it interesting that diet was attributed to the increase in developmental issues with the babies and medication wasn’t factored into that as a cause.
I’ve now just found out I’m almost 5 weeks pregnant and I’m so glad to have come across you and your book. You’ve made me feel comfortable in ignoring the medical advice given to me at the clinic on eating so many carbs in pregnancy but exasperatingly telling me to keep even tighter control of my bgls during this time. I plan on eating low carb but concentrating on good fats, proteins and hitting vital nutrients for baby to grow healthy. It’s just the start for me and hopefully in 8 months I’ll be holding my baby and my pregnancy has been a good one and doesn’t have to follow the typical pattern of one the hospital tells me it will. I want to avoid insulin if possible and be able to deliver and not have to necessarily have a c section at 37 weeks like they said. Thank you again, your book and advice is invaluable. I hope more of the medical community start to realise large carb consumption and low GI food promotion isnt the way for most people with insulin resistance to keep their limbs and manage their disease.
This is great information. I personally seem to be battling hypoglycemia (I’ve never got a reading over 90, even 1.5 hours after eating a bowl of oats, with a bunch of nuts, seeds, berries, and ghee). After my Fresh Test, my glucose was 60. Any thoughts on this? All I can find information about is HIGH blood sugar. Thanks so much!
I am so glad I found your books, Lily! I had pre-eclampsia with my previous (second) pregnancy and don’t want to endure that again. But, things aren’t looking good. I am 10 weeks with elevated protein urine (315mg) and my A1C came back at 5.7%.
Curious on testing for A1C. Is it best to be fasting? I wasn’t and I’m curious if that matters or not.
I have been trying my hardest to eat high protein/fat, lower carb and am at a loss as to why my labs are already presenting as concerning so early on. My OB is already pushing for low dose tylenol at 12 weeks.
Thanks for all you do!
Hello Lily, I am wondering what is the lowest recommended carb amount daily for a pregnant woman? I follow a low carb diet right now (I try to keep it below 50g per day with an occasional cheat day). When I was pregnant with my son and got the GD diagnosis, they told me I needed to be eating 30-45g of carbs per meal and freaked me out by saying that the baby needed carbs for brain development. Because of this, I ate more carbs and ended up on metformin and insulin. I’d like to avoid this if possible with my next pregnancy. So how many carbs are actually needed for normal fetal growth and development? Thank you
Before my pregnancy at in the first few weeks I always ate high-fiber, high-protein and relatively low carb. But in the past few weeks of my pregnancy (I’m 11 weeks now) this has been so difficult with aversions and nausea. I have had to eat more carbs and even more sugar than usual. The nausea is much better now though. I’m so worried because it seems the first trimester is so important in terms of lowering your chances of GD. Does anyone know if I start to eat better now that my nausea and aversions are abating do I have a better chance of avoiding GD? 🙁