This is not the first time I’ve written (or spoken) about the problems that plague conventional prenatal nutrition guidelines. Sometimes I feel a bit like a broken record, but judging by the questions that come my way from clients and from colleagues, I clearly need to talk about this more.
In this post, I’ll cover a handful of specific examples of how our conventional nutrition guidelines fall short for pregnant women. I specify a handful because there are many, many, many more issues that need attention—more than can be adequately covered on a blog (hint: you need a whole book to do it justice).
Research is constantly evolving, especially in the field of nutrition, and yet, there’s a lag time between new evidence getting incorporated into public policy. I’ve seen it firsthand. It’s unfortunate, but it’s the reality. No matter how great the program is and how good the people are, it takes an almost insurmountable amount of energy, effort, and most of all, TIME, to shift strongly-held beliefs. (And not to mention, the conflict of interest when corporations that have food-like products or medications to sell see their profits at stake with a change in such policies.)
Often, the battle of getting new information out into practice can take decades. Take, for example, trans fats. Researchers were speaking out against the use of trans fats starting in the 1960’s (if not sooner), and yet trans fats were not required to be labeled on food products (via the nutrition facts label) until 2006! Meanwhile, millions of people who were diligently following doctor’s orders to use margarine instead of “artery-clogging” butter were unknowingly setting the stage for heart disease, diabetes, and cancer.
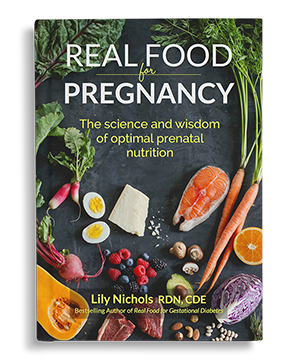
I’ve been scouring the pregnancy nutrition research for years, particularly in the past year+ (as I was researching for my book, Real Food for Pregnancy) and have discovered a wide gap between current prenatal nutrition policies and the latest evidence-based research.
Here are a few examples.
Why Prenatal Nutrition Guidelines Need to be Updated
Vitamin B12
If you look at any prenatal vitamin, you’ll see the”% daily value” listed to the right of every vitamin/mineral included in the formula. Most assume that as long as it says 100%, you’re set. You may be surprised to learn that recommended daily allowances (RDAs) are best-guesses and not set in stone. This is especially true for pregnancy, because most RDAs were set using data from adult men and then adjusted via mathematical estimations.
Or to put it this way:
“Nutrient requirements during pregnancy are usually calculated by adding an increment to the value for nonpregnant and nonlactating women that covers the cost of fetal growth and development and the associated changes in maternal tissue metabolism. This factorial approach, however, may not necessarily be correct because it does not take into account metabolic changes in absorption or excretion.” (American Journal of Clinical Nutrition, 2000)
Don’t get me wrong, the RDAs are still a good ballpark goal, but they aren’t perfect. When it comes to vitamin B12, the latest data suggests that pregnant women need TRIPLE the current recommended amount. (Journal of Nutrition, 2015)
This could be a significant concern for women who do not eat foods rich in vitamin B12 and/or rely entirely on a prenatal vitamin to meet their needs for vitamin B12 (such as vegetarians or those who limit foods of animal origin). B12 is one of many nutrients where *actual* needs are now known to be higher than current estimates.
Salt
Ever wonder why so many pregnant women crave pickles and olives? It’s probably the salt. Why? Because salt is an essential nutrient. I repeat: salt is an essential nutrient.
When you’re pregnant, your body has more fluids on board (blood volume expands + amniotic fluid) and when you have more fluids, you need more salt to balance it out. Think about it for a minute. If you’ve ever received IV fluids at the hospital, did they give you plain water? NO! They give you salt water because all of your bodily fluids also contain salt, where it serves as an electrolyte (among many other functions).
Many women are told to restrict salt (or they certainly are not told to eat more of it) as a means to avoid fluid retention or high blood pressure, but neither of these suggestions are scientifically sound. A Cochrane review—a highly respected source of evidence-based analyses—concluded that advice to lower salt intake in pregnancy should not be recommended. This advice holds true even for women who have high blood pressure or preeclampsia (some research suggests that more salt, NOT LESS, is ideal in these situations).
In fact, restricting salt can have serious consequences, such as growth restriction in baby and even fetal loss.
As one researcher explains,
“Salt is one of the integral components for normal growth of fetuses. Salt restriction during pregnancy is connected to intrauterine growth restriction or death, low birth weight, organ underdevelopment and dysfunction in adulthood probably through gene-mediated mechanisms.”(Journal of Biomedical Science, 2016)
And another,
“Extra salt in the diet seems to be essential for the health of a pregnant woman, her fetus, placental development, and appropriate function.” (Journal of Reproductive Immunology, 2014)
I’ve written about myths about salt in the past (see this article), and pregnancy is no exception. I could go on and on about this, but I cover all the relevant research on this topic in Chapters 2 and 7 of my book, Real Food for Pregnancy. The short answer is that salt is nothing to fear during pregnancy and, perhaps surprisingly, there are legitimate concerns about not getting enough salt.
Choline
Choline is still a new kid on the block in the nutrition world. Suggested intakes for choline were not set until 1998. If it had been discovered in the early 1900s, it would have been named something like “vitamin B45.” Originally studied for its role in liver function, choline is now well known to affect methylation, help prevent neural tube defects (alongside folate), and improve brain development.
The recommended intake for choline is higher during pregnancy (and even more so during breastfeeding), but these levels may not be enough. The latest data suggests that choline intakes TWICE that of current recommendations (930 mg vs. 450 mg) during pregnancy is optimal and is linked to higher cognitive function in infants, better placental function, and lesser chances of preeclampsia. (FASEB, 2013; FASEB, 2017)
This is great to know, but not exactly good news for conventional guidelines that suggest women avoid the most valuable source of this nutrient: liver. They also shy away from including the second-best source in sufficient quantities: eggs.
If you read through the Academy of Nutrition and Dietetics’ sample meal plan for pregnancy, the only eggs you’ll find are in the teeny tiny amount of low fat mayonnaise on the sandwich at lunch. Choline is found in a variety of foods other than eggs and liver, but in much lower quantities (we’re talking 115 mg in an egg yolk vs. 30 mg in ½ cup of cauliflower—and cauliflower is lauded as a good vegetarian source of choline as most other veggies have maybe 10 mg per serving, at best). Their meal plan barely squeaks by on choline needs and is nowhere close to the 930 mg that new research suggests in optimal.
Already, fully 94% of women do not meet the daily recommended intake of choline. (Journal of the American College of Nutrition, 2016) If the current guidelines were really up-to-date, they would, at the very least, highly encourage the consumption of eggs. Egg eaters have, on average, double the intake of choline when compared to non-egg eaters. My guess is that old—and unfounded—fears surrounding cholesterol are part of the hold up.
For more on why eggs are such an incredible food for pregnant women, read this.
Want to learn more about choline and pregnancy? See this in-depth post on the health benefits of choline for pregnancy.
Macronutrients
Conventional prenatal nutrition guidelines reflect government dietary guidelines; you know, the ones that push a high-carb, low-fat diet with 9-11 servings of carbohydrates, “half your grains whole,” and limited amounts of meat. This advice unfortunately does not reflect the last 3+ decades of research.
For one, the nutrients most commonly lacking in prenatal diets (such as choline, vitamin B12, DHA, and iron) are naturally the ones that contain protein and fat. If you’re to try and meet the macronutrient requirements in the current guidelines (45-65% carbohydrates), it’s very hard to “meet your macros” and also obtain enough of these nutrients from food alone.
Second, protein requirements during pregnancy are higher than we previously thought. Conventional nutrition guidelines suggest an estimated average protein requirement of 0.88 g/kg, or about 60 g of protein per day for a 150 lb woman. However, this recommendation is not as evidence-based as we would hope, as it relies primarily on data from nonpregnant adults. In fact, only a single protein requirement study of pregnant women was considered when setting this recommendation. (Institute of Medicine, 2005)
In 2015, the first-ever study to directly estimate protein needs in pregnant women was completed. Actual protein needs were found to be 39% higher in early pregnancy (defined as less than 20 weeks by this study) and 73% higher in late pregnancy (after 31 weeks) when compared to current estimated average requirements. (Journal of Nutrition, 2015)
The take home message from this research is that your body’s demand for protein “increases steadily as pregnancy progresses.”
Third, a high-carbohydrate diet is not the best option for women with higher blood sugar. Given the current state of affairs in the US, 49-52% of adults have either diabetes or prediabetes (most undiagnosed), so suggesting that all women eat a high-carbohydrate diet in pregnancy (i.e. one that raises blood sugar) is not best practice. (JAMA, 2015)
For example, researchers at Stanford University have shown that elevated blood sugar (far below the diagnostic threshold for gestational diabetes) is linked to a significantly higher risk of congenital heart defects. (JAMA Pediatrics, 2015) In a different study, high insulin levels (your body’s response to high blood sugar) in early pregnancy were linked to a significantly higher risk of neural tube defects. (Epidemiology, 2001)
Higher carbohydrate diets may also set women up to gain too much weight during pregnancy and may even have a carryover effect on their children’s propensity for obesity later in life.
For example, higher levels of obesity have been observed among infants and children exposed to this level of carbohydrate intake (52% of calories) in utero, even among healthy weight mothers eating within or below their estimated calorie needs. (American Journal of Clinical Nutrition, 2017)
I’m not saying (and have never said) that women shouldn’t eat any carbohydrates; they just shouldn’t be half of the diet for most women. At the very least, advice to make “half your grains whole” should be retired. When you look at micronutrient intake among pregnant women, those eating the most high-glycemic carbs have the lowest micronutrient intake. (American Journal of Clinical Nutrition, 2015)
We can do better.
If we want to give pregnant women the best chance of having a healthy pregnancy and a healthy baby, we desperately need to get better, more up-to-date, and scientifically sound advice out there.
I had a hard time hitting ”publish” on this blog post because it just scratches the surface of the myriad of reasons why prenatal nutrition guidelines need to be updated.
I’ve spent hundreds of hours reading research paper after research paper piecing together where we went wrong, why, and how we can do better. Thousands of research papers later, more than a year of writing, and a lot of breast milk, sweat, and tears, I’m excited to let you know that I’ve finally finished my second book, Real Food for Pregnancy.
Other areas that are beyond this post, but relevant to this discussion: omega-6 to omega-3 ratio, glycine needs, saturated fat, food safety (do you really have to swear off sushi and runny eggs?), fish vs. mercury debate, liver (does it really risk vitamin A toxicity?), vegetarian/vegan/plant-based diets, artificial sweeteners, alcohol, caffeine, pesticide residues and environmental toxins, advice on supplements, and much, much more.
Real Food for Pregnancy lays out all the evidence—over 930 citations—that supports a nutrient-dense, real food diet during pregnancy for optimal health of both mama and baby. It also delves deeply into all of the above controversial topics, so you can make a truly informed decision about your food and lifestyle choices.
Here’s what a few smarties are saying about it:
“No one has dissected the research on prenatal nutrition—and done so in the context of ancestral diets—to the depth that Lily Nichols has in Real Food for Pregnancy. If you want an evidence-based rebuttal to the outdated prenatal nutrition guidelines, look no further.”
—Robb Wolf, 2x NYT Bestselling Author, Wired to Eat & The Paleo Solution
“Real Food For Pregnancy should find its way into every medical school and prenatal clinic. Lily Nichols’ first book, Real Food for Gestational Diabetes, is a staple in my teaching here at West Virginia University and has shifted how many in our department view nutrition. Her second book is encyclopedic; it’s amazingly well-referenced and more in-depth than many textbooks. If mothers embrace Lily’s advice, the next generation will hopefully suffer less obesity and diabetes.”
—Mark Cucuzzella, MD, FAAFP, Professor at West Virginia University School of Medicine
“As a practicing CNM (midwife) for almost 30 years, I am thrilled to have found Lily’s writing and expertise. Real Food for Pregnancy is one that we’ll keep in stock at our clinic and will teach from during our early pregnancy classes. I really enjoyed the descriptions of the vitamins and minerals and how to get them from food. In my experience, too many people believe that prenatal vitamins will solve all of their problems or will guarantee the health of the baby.”
—Cheryl Heitkamp, APRN, CNM, President of Willow Midwives in Minneapolis, MN
“Real Food for Pregnancy should be considered essential reading for any woman who is currently pregnant or planning conception in the near future. I have not found a similar text with the breadth and depth of discussion on prenatal nutrition. What sets Real Food for Pregnancy apart is how it logically explains the current scientific evidence that is disrupting modern nutrition science and pushing conventional dogma into a new direction. Lily Nichols’ meticulously cited text provides not only a quick read but also plenty of details and references for those who wish to dig further. This book may very well serve as the tipping point leading to a sea change in nutrition science and medical care. I will be recommending it to my patients within my busy high-risk obstetrics practice.”
—Amit Bhavsar, MD, Board certified Obstetrician-Gynecologist practicing outside of Austin, TX
Learn more…
If you’re interested to learn more, Real Food for Pregnancy is available for purchase on Amazon (PRINT or KINDLE).
Read the first chapter for FREE!
Curious to learn more about the book before buying? You’re in luck!
I’m giving away the first chapter for FREE over at www.realfoodforpregnancy.com.
In this excerpt from the book, you’ll see a side-by-side comparison of the nutrient breakdown from one of my “real food” meal plans and the conventional one. Can you guess which one is more nutrient dense? (hint, hint)
If you agree that prenatal nutrition guidelines need to be updated, you’ll definitely want to read this.
Happy reading!
Until next week,
Lily
PS – Did you catch that?
Real Food for Pregnancy is available on Amazon:
Read the first chapter 100% for free. It’s my gift to you (and the next generation). Get it here.



I’ve had my doubts about prenatal nutrition guidelines, but haven’t had the time or energy to thoroughly research all of the above topics in enough detail. I’ve pre-ordered real food for pregnancy and look forward to reading. Thanks for doing what you do, Lily! I, for one, am a dietitian that’s ready to do better for my prenatal clients.
Appreciate your support, Ann!
This is excellent Lily! I can’t wait to read the whole book!
Thanks April!
You’re the first person I’ve found that talks about the salt in pregnancy issue. I always craved salt like crazy during pregnancy and it now makes so much sense. When I didn’t give in, my blood pressure would go UP, not down.
I can’t wait to read that section of your book. Any chance you can publish it early?!?! hint, hint.
The research on salt is very, very interesting and, frankly, opposite of what most healthcare providers are told. It’s pretty clear that a low salt diet has no place in prenatal guidelines.
Lily,
Wow! I just finished the book, and let me tell you, I think this is excellent work! I had just finished reading Nina Planck’s books on real food in search of a new set of dietary ideals. I wanted to transition out of veganism (which spanned about 7 months) as I’m confident was hindering my fertility. I’ve been following your recommendations for nutrition, trying to heal my body from my previous well-intentioned change in diet. I feel so much better and am so elated to have stumbled across your new book before continuing to be frustrated with my body any longer or becoming pregnant again. I’ve already seen improvement and wanted to thank you for your frankness about vegan/vegetarian diets in pregnancy (with the data to back it up). I kind of hate recipes in cookbooks, but yours are all home runs. I’d love to see a full cookbook with equally simple and delicious recipes!
Thanks again!
Appreciate the feedback, Melissa! So glad the section on vegetarian/vegan diets during pregnancy was helpful! I initially didn’t include this in the book, but the more data I read, the more I felt it was an important topic to directly address.
Your book so far is fantastic! However, the prenatal vitamin website you sighted on page 89 is not working! Please advise where I can find the list, as my wife’s current supplement doesn’t seem to be adequate. Thank you!
All is working. Please try again!
I had NO IDEA about glycine. This is fascinating. I can’t wait to read your book!
Hi Lily! Your research is always so fascinating to me. I know you’re not one to prescribe very specific numbers to macronutrients as you emphasize eating intuitively, but do you have general recommendations for the ratio of carbs to protein to fats that a woman should be aiming to eat during pregnancy? There is so much noise out there, and I value the research you’ve done on these topics! Also, I ordered your book–so, so excited for it to arrive! Keep up the amazing work!
I love all your articles and your book, Lily. Thank you so much!
I am currently trying to lose weight while also preparing my body for another pregnancy. I try my best to follow the Weston Price Foundation recommendations but I am really considering using the Seeking Health Prenatal in my next pregnancy to fill the gaps. Do you recommend starting the prenatal in the preconception period or just focusing on nutrient dense foods during this time?
Thanks!
I would be interested to hear your recommendations for the most complete prenatal vitamin on the market.
There’s a link included in Ch 6 of Real Food for Pregnancy to my recommendations. I don’t print them directly in the book so that I can update them as formulations change or new products come on the market.
What type of prenatal vitamin do you recommend taking? I need something I can order off Amazon Prime.
There’s a link included in Ch 6 of Real Food for Pregnancy to my recommendations. I don’t print them directly in the book so that I can update them as formulations change or new products come on the market.
Also, see my Instagram story highlights called “supplements”. https://www.instagram.com/lilynicholsrdn/
The web site is not found that is listed in your book!!!!
Never mind sorry i must have had it typed in wrong, I got the list and I love the details with pros and cons!
Hi there,
I’m part way through listening to Real Food for Pregnancy on audible and finding it super helpful. Thanks! One problem though is I don’t seem to have access to the pdf downloads you mention with the meal plans and list of healthy drinks. Are you able to send these to me please? Happy to provide evidence of my audible download if you need it?
Thanks so much in advance,
Pamela (leicestershire, england)
Hi Pam,
Glad you’re enjoying Real Food for Pregnancy!
If you purchased the audiobook on Audible/Amazon, the pdf download is located in your Audible account. Please see this link for instructions. https://audible.custhelp.com/app/answers/detail/a_id/5046/~/how-can-i-download-the-pdf-that-comes-with-my-audiobook%3F
I love all your articles and your book, Lily. I’m learning so much, Thank you!!! I’ve been looking at your list of recommended prenatal vitamins, but it looks like there are only available in America. Do you have any suggestions for best prenatal vitamins on the market in Australia? All GPs I have spoken with recommend Elevit, which from reading your book doesn’t seem to be great. Folic acid, high iron, only 1 tablet per day etc
Would really appreciate any help or direction
I loved your book Real Food for Pregnancy!
The non stick chapter has really concerned me. I am in the process of changing now, but I used non stick in the early stages. Also in your book it says it can take up to four years to leave your body. Am I too late to make a difference?
Hello! I’m reading your book at the moment, and loving it. The thing I’m struggling with is trying to ensure I’m hitting the increased targets for my micro nutrients. I know you talk about the plate technique and that it’s not about using trackers, but I’d like to look at my current diet to see where my gaps are. I’ve spent hours flicking back and forth with your book trying to work out what my targets should be. Do you possibly have anything like the RDA chart but updated with all the research you have done? In your book you say things like needing triple current RDAs for B12, so I am able to set targets there, but this is proving hard for other things. I’d love some help in this just to start me off on my more mindful food journey!
I’d love to see this too!
I’m currently reading your book and learning so much ! Thank you! I have a question about taking liver pills. I read somewhere else that if you take liver pills you do not need to take a prenatal?
It’s hard to keep up with the changes of prenatal vitamins and what is popular at the time. Do you have favourites you recommend?
What are your thoughts about taking wheatgrass juice powder supplementation during pregnancy and breastfeeding? Like Dr. Berg’s product?
Thanks!
Hi Lily,
I recently watched a documentary called “What the Health.” It states how dioxin is very toxic and is found in meats – even organic /grass fed meat and animal products. These are two conflicting ideas from what you presented and what the documentary has presented because I was following the diet advice you gave in your book.
Do you know the effects of Dioxin and is it as bad as the documentary says for pregnant/breastfeeding women – it states that the only way we can get rid of dioxin in our bodies is through the placenta and when breastfeeding and has scared me from eating meat, but I also highly value your advice and book too.
Thanks a lot!
Absolutely love your book. Listening to it on audible second time in a row. Do you offer any consultation?
Hello,
I have been reading your book and loving it. I’m 5 weeks pregnant, its at 7 weeks that nausea strikes and hopefully doesn’t stay this time. I’ve been doing my best to eat eggs and salmon while I still can:)
My question is about nitrates. You seem to be a fan of eating deli meat, but I don’t hear and haven’t found anything about avoiding nitrates in your book. Wondering if you could weigh in on that? I would love to be able to eat lunch meats.
After being prescribed a glucose meter to monitor my borderline GD and being told to consume 40% complex carbs at the same time, I had the hardest time trying to actually keep my blood sugar lower than before the 40% recommendation. It just didn’t make any sense. I was spiking, crashing and eating more during the day but none of it the right foods. I told my husband the doctor is just flat wrong. The math didn’t check out…how was I supposed to consume up to 200g in carbs?! I found your book and finally got confirmation that the outdated advise was actually giving me GD!
Hi Lily, I just found out I’m pregnant and I have your book. I am suffering from information overload at this time, and I wondered if there is a summary chart on nutrition for pregnancy anywhere in the book or blog? I’m working through the book but I’m a little panicked because I need to pick a prenatal asap